Breadcrumb
Pressure Support Ventilation
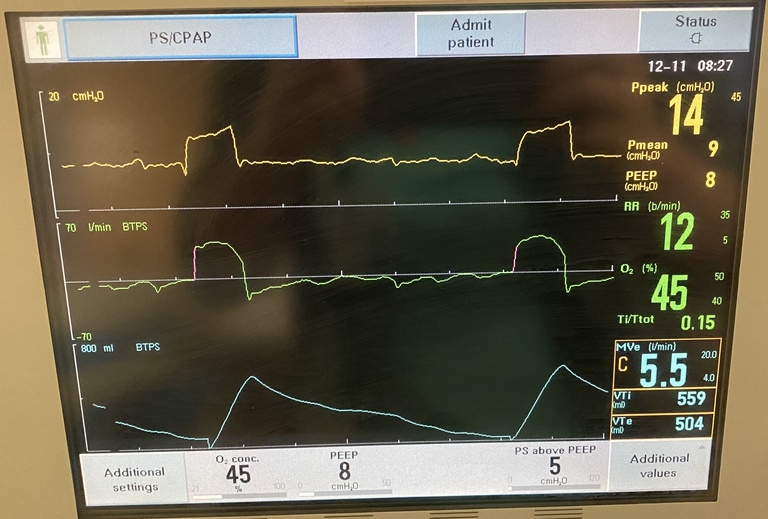
Pressure support ventilation (PS) is a form of positive-pressure ventilation. It is patient driven: every breath is initiated by the patient. It is triggered by either a change in pressure or a change in flow, both of which occur when the patient attempts to take a breath on their own. Once the breath is triggered, the ventilator provides additional pressure support throughout inspiration in addition to whatever the patient is able to produce on their own (this helps overcome the resistance of the endotracheal tube etc). A cycling value determines when the pressure is decreased, in order to transition from inhalation to expiration; typically this is done when flow has dropped by a certain value below peak flow (e.g., 25%) or flow has decreased beyond a certain minimum rate (e.g., 5 L/min).
Pressure support ventilation requires an intact respiratory drive, since the ventilator will not provide any breaths beyond what the patient initiates. The patient is responsible for their own breathing in PS: thus, it is not good for deeply-sedated patients or those with otherwise impaired mentation. Pressure support is useful for patients who have good respiratory effort and mentation i.e. those who may be candidates for successful extubation. A patient who is breathing comfortably, hemodynamically stable and mentating well on PS and requiring low FiO2 and PEEP may be ready to be extubated (see Ventilator liberation section for more details).